Because Pores in These Areas Produce More Skin Oil
The Essential Info
Although acne lesions can appear anywhere on the body except the palms of the hands and soles of the feet, they occur most often on the face and upper body. This is most likely due to the following factors:
More Skin Oil: The skin on the face and upper body contains more, and larger, skin oil glands compared with other parts of the body, and these glands produce more skin oil than elsewhere on the body. More skin oil normally leads to more acne.
Higher Male Hormone Levels: Many people don’t realize that the skin contains hormones. Higher amounts of androgens (male hormones that are present in both males and females) in the skin of acne-prone areas such as the face and upper body may further contribute to the development of acne in these areas.
More Acne Bacteria: Acne bacteria lives and multiplies in skin oil. Since the face and upper body have more, and larger, skin oil glands, more bacteria can fester in these areas.
Over-accumulation of Skin Cells: When skin cells accumulate, they can block a pore and begin the process of an acne lesion forming. For unknown reasons, this happens more frequently on the face and upper body.
More Inflammation: Acne is an inflammatory disease, and the skin of the face and body may be more susceptible to inflammation.
Lower Skin Acidity: Acne bacteria prefers a less acidic environment, and the skin of the face is less acidic compared to other parts of the body.
The Science
- More, and Larger, Sebaceous Glands (Skin Oil Glands)
- Higher Male Hormone Levels
- More Acne Bacteria
- Over-accumulation of Skin Cells
- More Inflammation
- Higher Skin pH
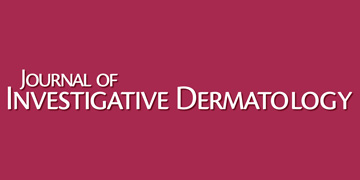
Some areas of the skin are more prone to acne than the skin on the rest of the body. These include:
- Face
- Back of the neck
- Upper back
- Chest
- Shoulders/Upper arms1-15
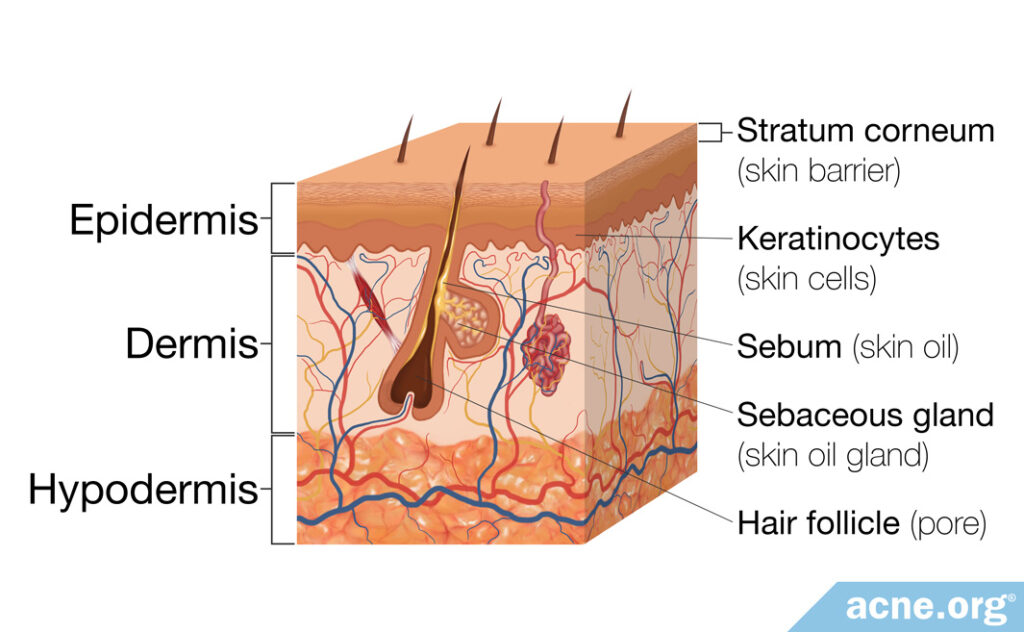
To understand why certain areas of skin are prone to developing acne, let’s begin with a quick review of the skin’s structure. The skin covering the human body is made of three layers.
- The outer layer is called the epidermis
- The middle layer is called the dermis
- The deepest layer is called the hypodermis2,3
Now let’s look more deeply at the biological reasons that some areas of skin are acne-more prone than others.
More, and Larger, Sebaceous Glands (Skin Oil Glands)
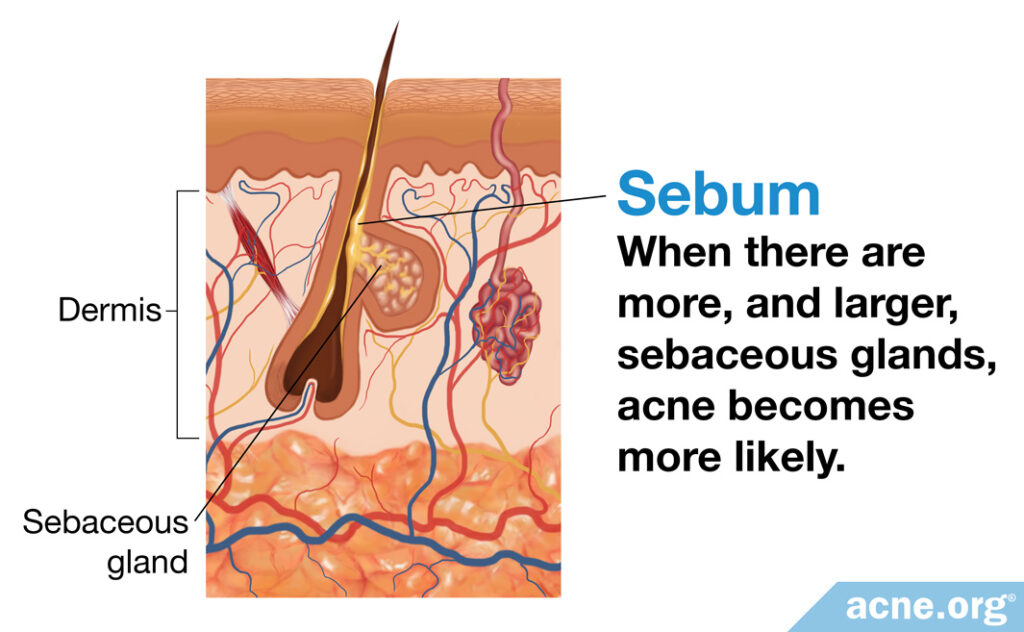
The middle layer of the skin, the dermis, contains skin oil-producing glands called sebaceous glands. These glands produce sebum (skin oil), that performs multiple functions for the skin.4
Research shows that most individuals with acne have larger sebaceous glands on their facial skin than individuals without acne.5 And since the sebaceous glands are larger, this means they produce more sebum.
Scientists don’t fully understand the role of sebum in acne formation, but they hypothesize that the sebum produced by sebaceous glands increases inflammation around pores, leading to clogged pores and acne lesions.6
Sebaceous glands exist on all areas of the body except the palms of the hands and soles of the feet, and are found in the highest concentrations on the face, forehead, and on the scalp. The area with the highest concentration is the T-zone, which includes the forehead, the bridge of the nose, and the fold between the nose and the lips. The T-zone has as many as 400 to 900 glands per square centimeter.1,4,5
Sebaceous glands are also numerous on the back of the neck, upper back, chest, and shoulders, which are areas where body acne commonly forms.
In addition to enlarged sebaceous glands in acne-prone areas of the skin, it is possible that the composition of sebum produced by acne-affected skin is different from that which is produced by non-acne-affected skin. One study found that skin with acne produces sebum containing a larger amount of certain fats and oils compared to skin without acne.7
Expand to read details of study
A 1970 study published in the Journal of Investigative Dermatology examined 65 specimens of sebum from the face, neck, chest, and backs of men and women with acne. The authors confirmed a difference in composition, demonstrating that sebum from skin with acne has more substances called free fatty acids and triglycerides.7
Higher Male Hormone Levels
Hormones course through our veins in our blood, and also reside in our skin.
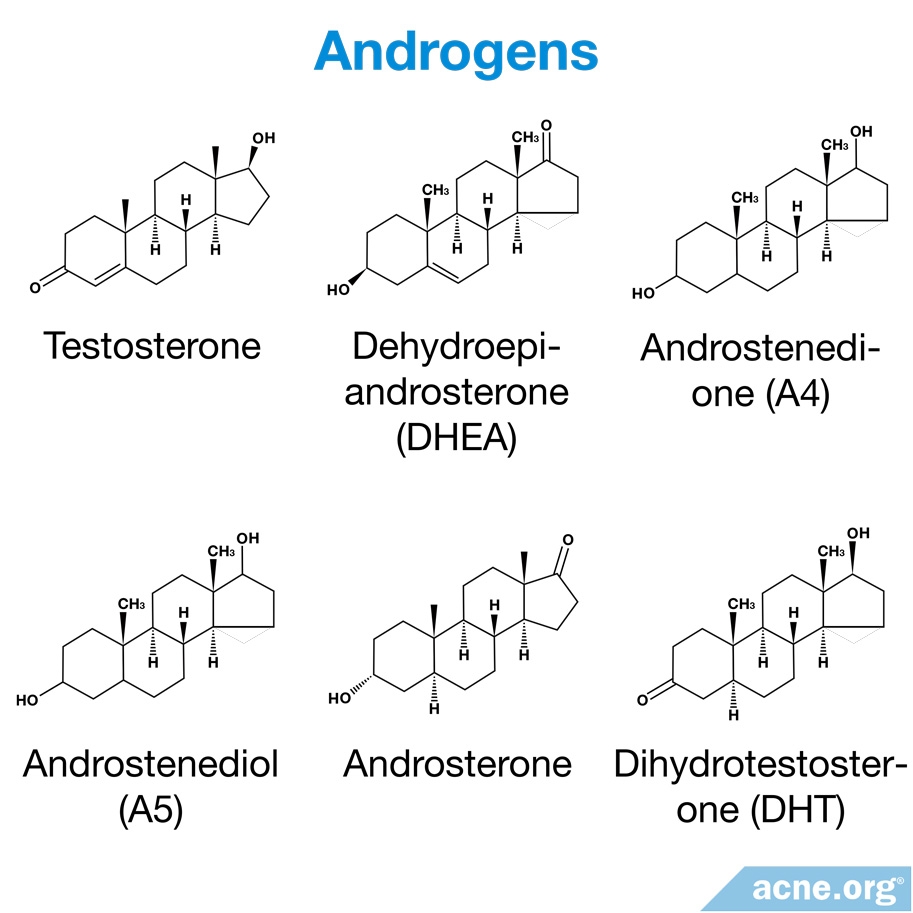
We know that both males and females with acne tend to have higher androgen (male hormone) levels in the blood,8,9 but that doesn’t explain why acne occurs most often on the face and upper body. The explanation starts to become clearer when we look at hormone levels inside the skin itself. As it turns out, acne-prone skin areas also tend to contain higher amounts of androgens.
How do androgens get into the skin? The skin has enzymes that convert androgens in the blood to forms of the hormone that are active in the skin. An example of one of these hormones is dihydrotestosterone (DHT). DHT attaches itself to receptors in the sebaceous glands, causing them to enlarge and increase sebum production.10-12,16 Increased sebum production is then associated with acne. A 1971 study describes this process.12
Expand to read details of study
In a 1971 study published in the Journal of Investigative Dermatology, researchers examined skin specimens taken from 32 individuals. Samples were taken from individuals with and without acne and from affected and unaffected skin. The results showed that skin with acne produced 2 to 20 times more DHT than normal skin. The study showed also that the rate at which the skin created DHT from the androgen, testosterone, in the bloodstream differed depending on the location of the skin. The face and the upper back – common locations for acne – converted testosterone to DHT at higher rates than skin on other parts of the body. These results suggest that skin exhibits acne-prone characteristics because of the rates at which it processes androgens in the bloodstream.12
More Acne Bacteria
Normal skin contains a variety of microorganisms, such as bacteria. As we have learned, acne-prone skin areas, such as the face, neck, and upper back, have a high density of sebaceous glands and produce more sebum. For this reason, these areas tend to host organisms that can feed on sebum. An example of such an organism is C. acnes, the bacteria known to contribute to the redness and soreness of acne. In fact, C. acnes is the dominant bacteria in acne-prone skin areas where there is a high density of sebaceous glands.17,18
Another microorganism that co-exists with C. acnes on human skin, especially in acne-prone areas, is Malassezia. Malassezia is a fungal organism responsible for “stubborn” (persistent) acne. This organism changes the composition of sebum, which might lead to skin cells accumulating and clogging pores.19
Over-accumulation of Skin Cells
When skin cells accumulate and fail to shed from the skin as they should, they can clog the pore and contribute to acne formation. For unknown reasons, this happens more often in the pores of the face and upper body.
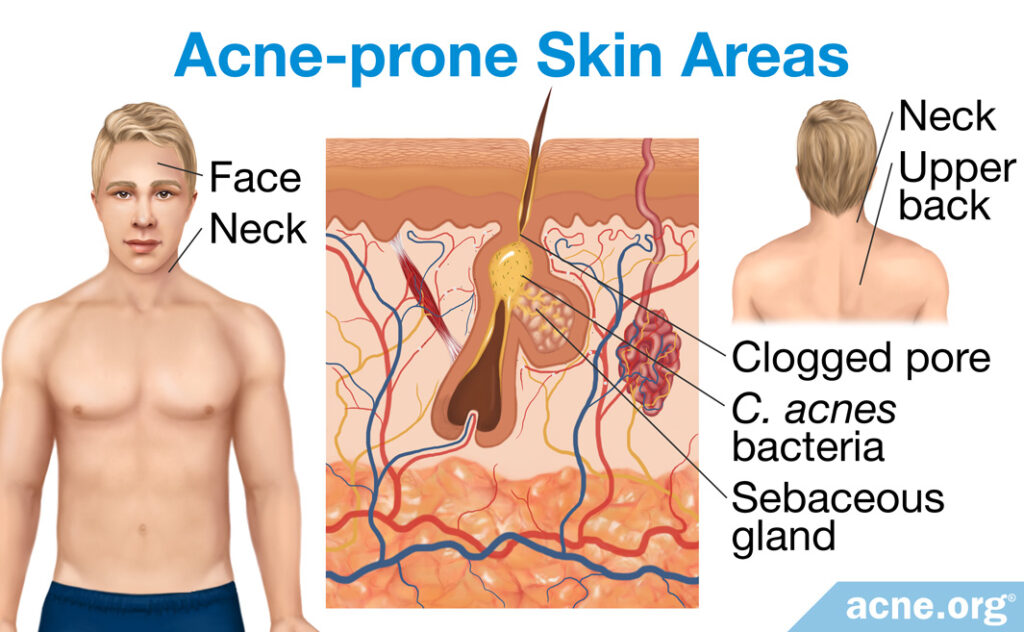
The stratum corneum is the outermost layer of skin – the topmost layer of the epidermis. The purpose of the stratum corneum is to form a barrier to protect underlying tissue from infection, dehydration, chemicals, and abrasion. It is made of dead skin cells called corneocytes, which start out as live cells called keratinocytes that are formed at the base of the skin. These keratinocytes slowly move up toward the surface and die, becoming corneocytes, and eventually shed off in a process called desquamation.
In normal skin, it takes about 2 weeks for keratinocytes to form, move up into the stratum corneum, and shed from the skin. However, skin cells are over-produced in acne-prone skin areas, and it can take twice as long for these cells to reach the surface and shed. This slowdown can clog pores and cause acne to form.14
In addition, research suggests that people with acne tend to have a weakened skin barrier. The stratum corneum, which forms the skin barrier, is thinner on the face compared to other parts of the body. In other words, the face may be the “weak link” in terms of the skin barrier, which may explain why it is often the first area to develop acne.14
More Inflammation
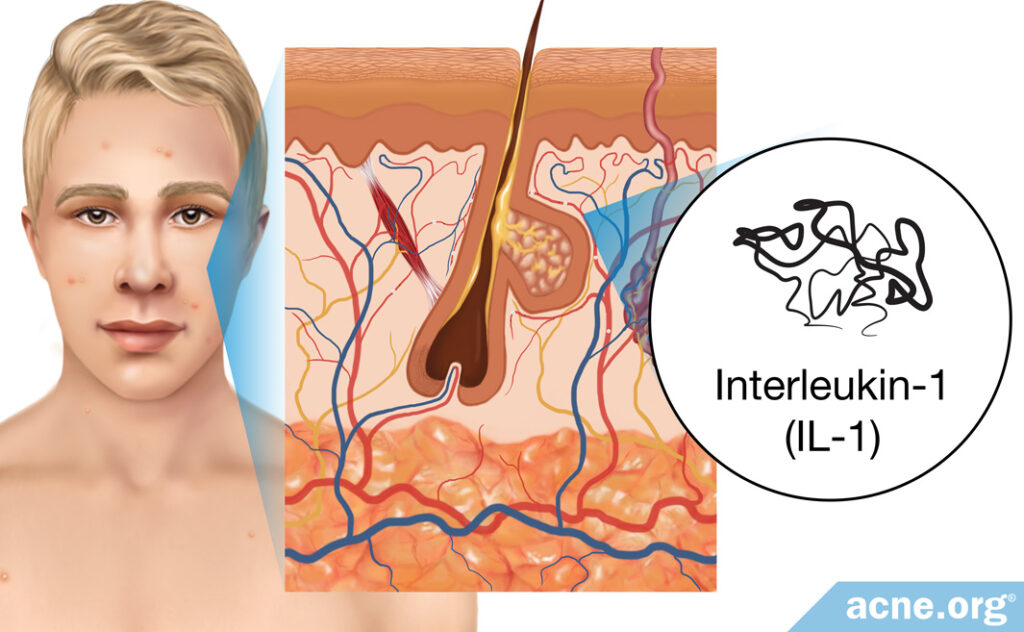
Scientists believe that acne is, at its core, an inflammatory disease. Research shows that inflammation associated with an immune substance called interleukin-1 (IL-1) may be central to the development of acne.
A recent study found that acne-prone areas of the skin like the face and upper body may be more sensitive to interleukin-1 than other areas of the skin and may therefore be more likely to develop inflammation and acne.15
Expand to read details of study

In a 2013 study published in The Journal of Clinical and Aesthetic Dermatology, researchers looked at the number of interleukin-1 receptors in the skin on different parts of the body. The results showed that the epidermis of the face and upper arms had elevated levels of interleukin-1 receptors. This may help to explain why these acne-prone areas of the skin may be more easily inflamed and more likely to develop acne.15
Higher Skin pH
The pH of the skin refers to its acidity and is measured on a scale of 0 to 14. The skin’s pH matters because bacteria such as C. acnes prefer a higher (less acidic, more alkaline) pH.20 It turns out that the pH of the skin on the face is higher compared to the skin of the chest and back, making the face a friendlier environment for acne bacteria.21 This may be another reason why acne is more likely to develop on the face before other parts of the body.
Interestingly, one study found that people with acne tended to have a higher pH overall compared to people without acne.22
References
- Ebling, F. J. The sebaceous glands. J. Soc. Cosmetic Chemist. 16, 405-411 (1965). http://journal.scconline.org/abstracts/cc1965/cc016n07/p00405-p00411.html
- Arda, O., Goksugur, N. & Tuzun, Y. Basic histological structure and functions of facial skin. Clin. Dermatol. 32, 3 – 13 (2014). https://www.researchgate.net/publication/259244780_Basic_histological_structure_and_functions_of_facial_skin
- Amirlak, B. Skin anatomy. https://emedicine.medscape.com/article/1294744-overview
- Makrantonaki, E., Ganceviciene, R. & Zouboulis, C. An update on the role of the sebaceous gland in the pathogenesis of acne. Dermatoendocrinol. 3, 41 – 49 (2011). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3051853/
- Thiboutot, D. & Del Rosso, J. Q. Acne vulgaris and the epidermal barrier: Is acne vulgaris associated with inherent epidermal abnormalities that cause impairment of barrier functions? Do any topical acne therapies alter the structural and/or functional integrity of the epidermal barrier? J. Clin. Aesthet. Dermatol. 6, 18 – 24 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23441236
- Kellum, R. E. & Strangfeld, K. Acne vulgaris. Studies in pathogenesis: fatty acids of human surface triglycerides from patients with and without acne. J. Invest. Dermatol. 58, 315 – 318 (1972). https://www.sciencedirect.com/science/article/pii/S0022202X15481412
- Nicolaides, N., Ansari, M. N., Fu, H. C. & Lindsay, D. G. Lipid composition of comedones compared with that of human skin surface in acne patients. J. Invest. Dermatol. 54, 487 – 495 (1970). https://core.ac.uk/download/pdf/82778461.pdf
- Shaw, J. C. Acne: effect of hormones on pathogenesis and management. Am. J. Clin. Dermatol. 3, 571 – 578 (2002). https://www.ncbi.nlm.nih.gov/pubmed/12358558
- Galobardes, B., Davey Smith, G., Jeffreys, M., Kinra, S. & McCarron, P. Acne in adolescence and cause-specific mortality: lower coronary heart disease but higher prostate cancer mortality: the Glasgow Alumni Cohort Study. Am. J. Epidemiol. 161, 1094 – 1101 (2005). https://www.ncbi.nlm.nih.gov/pubmed/15937017
- Ebede, T. L., Arch, E. L. & Berson, D. Hormonal treatment of acne in women. J. Clin. Aesthet. Dermatol. 2, 16 – 22 (2009). https://www.ncbi.nlm.nih.gov/pubmed/20725580
- Knutson, D. D. Ultrastructural observations in acne vulgaris: the normal sebaceous follicle and acne lesions. J. Invest. Dermatol. 62, 288 – 307 (1974). https://www.ncbi.nlm.nih.gov/pubmed/4361988
- Sansone, G. & Reisner, R. M. Differential rates of conversion of testosterone to dihydrotestosterone in acne and in normal human skin–a possible pathogenic factor in acne. J. Invest. Dermatol. 56, 366 – 372 (1971). https://www.ncbi.nlm.nih.gov/pubmed/4253995
- Blauer, M. et al. Location of androgen receptor in human skin. J. Invest. Dermatol. 97, 264 – 268 (1991). https://www.sciencedirect.com/science/article/pii/S0022202X9190102V
- Tagami, H. Location-related differences in structure and function of the stratum corneum with special emphasis on those of the facial skin. Int. J. Cosmet. Sci. 30, 413 – 434 (2008). https://www.ncbi.nlm.nih.gov/pubmed/19099543
- Tanghetti, E. A. The role of inflammation in the pathology of acne. J. Clin. Aesthet. Dermatol. 6, 27 – 35 (2013). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3780801/
- Sutaria, A.H., et al. Acne vulgaris. StatPearls, StatPearls Publishing, 1 August 2022. https://www.ncbi.nlm.nih.gov/books/NBK459173/
- Grice, E. A. & Segre, J. A. The skin microbiome. Nat. Rev. Microbiol. 9, 244 – 253 (2011). https://www.ncbi.nlm.nih.gov/pubmed/21407241
- Dréno, B. et al. The skin microbiome: A new actor in inflammatory acne. American Journal of Clinical Dermatology, 21(S1), pp. 18–24 (2020). https://doi.org/10.1007/s40257-020-00531-1
- Xu, H. and Li, H. Acne, the skin microbiome, and antibiotic treatment. American Journal of Clinical Dermatology, 20(3), pp. 335–344 (2019). https://doi.org/10.1007/s40257-018-00417-3
- Kuo, S. H., Shen, C. J., Shen, C. F. & Cheng, C. M. Role of pH value in clinically relevant diagnosis. Diagnostics (Basel). 10, 107 (2020). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7167948/
- Kim, S. A., Kim, B. R., Chun, M. Y. & Youn, S. W. Relation between pH in the trunk and face: Truncal pH can be easily predicted from facial pH. Ann. Dermatol. 28, 216‐221 (2016). https://pubmed.ncbi.nlm.nih.gov/27081270/
- Prakash, C., Bhargava, P., Tiwari, S., Majumdar, B. & Bhargava, R. K. Skin surface pH in acne vulgaris: Insights from an observational study and review of the literature. J. Clin. Aesthet. Dermatol. 10, 33‐39 (2017). https://pubmed.ncbi.nlm.nih.gov/29104722/
The post Why Do People Get Acne Mostly on the Face and Upper Body? appeared first on Acne.org.
