Hives, Also Known as Urticaria, Are Itchy Welts of Various Sizes on the Skin, and Are Not Acne

The Essential Info
Hives, also known as urticaria, are itchy, usually red or pink, welts of various sizes on the skin.
They develop usually within minutes of contact with an allergy trigger (i.e. a particular food, medication, animal, or substance), which causes the body to release a molecule called histamine under the skin.
Hives usually do not require medical attention and go away on their own within 1 – 2 days or less. If hives are causing itchiness or discomfort, over-the-counter antihistamines such as cetirizine (Zyrtec®), fexofenadine (Allegra®), or loratadine (Claritin®) can provide relief.
Anyone can get hives, but the following people tend to get them more often:
- Children
- Females between 30 and 60
- People with allergies
Chronic Hives: Sometimes hives can stay on the skin for longer periods of time (over 6 weeks), and at that point are called chronic hives. About one-half of cases of chronic hives are caused by the immune system attacking itself. In the case of chronic hives, daily antihistamine intake or an anti-inflammatory injectable prescription called Omalizumab (Xolair®) may be prescribed.

The Science
Hives, also known as urticaria, are itchy welts on the skin that normally appear red or pink on most skin types. According to the American Academy of Dermatology, welts can be “as small as a pen tip to as large as a dinner plate.”1
Hives usually develop suddenly and rapidly when a trigger makes the body release a molecule called histamine under the skin.2 Often, allergens like food, insect bites, and seasonal pollen are the trigger, but other things can be the trigger too, including infection, chronic illness, extreme temperatures, and more.
Hives usually do not require medical attention and clear spontaneously within 1-2 days or sooner.2
Anyone can get hives. About 20% of people get affected at some point in their life. Children, females between 30 and 60, and people with allergies get hives more often than others.3
Symptoms of Hives

Hives are slightly raised, usually pink or red, welts that can develop anywhere on the skin. They can appear as either just one single welt on the skin or as several welts in groups. Sometimes, several smaller neighboring welts will merge, covering larger areas of skin.
The welts are usually very itchy and can sometimes hurt or sting.
Hives usually disappear on their own in under 24 hours but may come back in a different location. All signs and symptoms usually clear on their own in a couple of days.
Sometimes hives do not go away within 2 days, and sometimes–not even within weeks. If hives stick around for 6 weeks or longer, they are called chronic (long-lasting).
Causes of Hives
Hives develop when a trigger of some kind makes the body release a molecule called histamine under the skin. Often, an allergen is the trigger, such as:
- Food:
– Dairy
– Eggs
– Fresh fruit, especially citrus
– Fish and shellfish
– Chocolate
– Peanuts - Medications, particularly:
– Oral antibiotics
– Pain killers - Insect bites
- Seasonal pollen
- Animals
- Latex
But sometimes a non-allergic factor is the trigger, such as:
- Infection (everything from the common cold to HIV)
- Chronic illness (e.g. lupus, vasculitis, or thyroid disease)
- Exposure to sunlight
- Extreme temperatures
- Physical exercise
- Emotional stress
Usually, symptoms develop within minutes after contact with the trigger. In some people, however, symptoms may take a few hours to become apparent.
Chronic Hives: The triggers of chronic (>6 weeks) hives are often difficult to identify. Allergy is rarely the cause.4 Up to half of all cases of chronic hives develop because the immune system attacks the body’s own tissues. Hives that are caused by the immune system attacking the body’s own tissues are called autoimmune hives.
We do not know why autoimmune hives develop, but we do know that they can accompany other autoimmune disorders, for example lupus and rheumatoid arthritis.
Other chronic conditions associated with a greater risk of chronic hives:
- Viral hepatitis
- Under- or overactive thyroid gland
- Intestinal helminths (parasitic worms)
Chronic hives tend to come and go. Certain factors can make symptoms worse, including:
- Heat
- Coffee
- Insect bites
- Emotional stress
- Tight clothing
- Alcohol
In about half of cases, chronic hives will subside on their own within 6 months. In the other half, hives continue to go away and come back.
Diagnosis
Normally, you do not need to visit a doctor for hives unless they are bothersome or do not clear within 48 hours. If you do consult a doctor, he will normally be able to easily identify the condition by closely looking at the affected skin. Tests are not usually required. However, if your hives are persistent, a doctor may prescribe test(s) to figure out what is causing them, such as:
- Blood tests
- A stool sample to rule out intestinal helminths
- An erythrocyte sedimentation rate test to assess the function of the immune system
- Thyroid function test to check the function of your thyroid gland
- Liver function tests to rule out hepatitis
When it comes to chronic hives, a blood test can help your doctor determine whether your own immune system attacking your tissues might be the culprit. The clue would be elevated levels of an antibody called IgG in your blood, which would suggest that the hives are autoimmune in nature.5
Treatment
Most cases of hives disappear on their own within 48 hours or less and do not require medical attention.
The best treatment is to identify and avoid triggers. For instance, if you notice that you get hives every time you eat peanuts, avoid eating peanuts. If itch is bothersome, oral over-the-counter antihistamines like cetirizine (Zyrtec®), fexofenadine (Allegra®), and loratadine (Claritin®) can help relieve the itch.3 It normally takes around 90 minutes for the antihistamines to begin relieving itch and swelling.
In more severe cases, your doctor may prescribe a short (up to 5 days) course of oral corticosteroids, usually prednisone.3
Two medications are approved by the U.S. Food and Drug Administration (FDA) for the treatment of chronic hives:
- Antihistamines: The first-line treatment, usually taken orally on a daily basis.
- Omalizumab (Xolair®): May be recommended when antihistamines have failed to work– usually administered through injection.
While these treatments work for many people with chronic hives, some people do not improve on the treatment for reasons that researchers still do not understand.5 In these cases, doctors tend to reach for alternatives such as drugs that suppress the immune system, like cyclosporine, or medications used to treat inflammatory diseases, like hydroxychloroquine, sulfasalazine, or colchicine.2
Extreme Hives: Angioedema
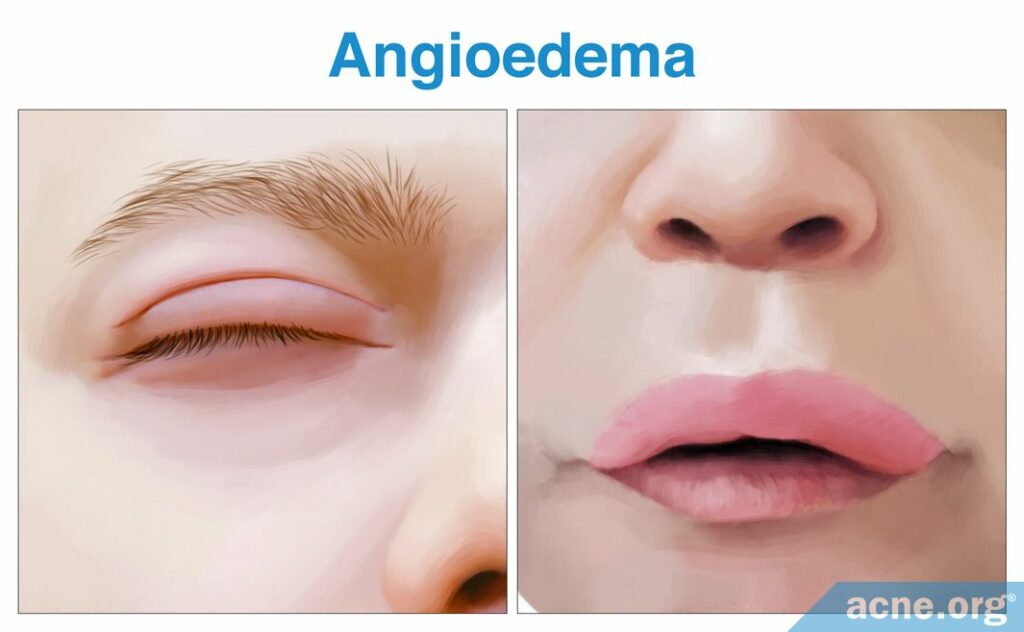
Angioedema (an-gee-oh-eh-dee-ma) is a medical term for a pronounced swelling that reaches deep into the skin, often caused by an allergic reaction. Angioedema occurs in approximately 40% of patients with chronic hives.5 It often involves the eyelids and the lips, but can involve other areas. If you think you are experiencing angioedema, call 911 immediately because you may need an injection of adrenaline. Angioedema may be one of the first signs of a severe life-threatening allergic reaction called anaphylaxis.
Hives Vs. Acne
Hives and acne are different, unrelated conditions. Acne is a disease that often requires treatment, while hives are usually harmless and disappear within a couple of days.
Hives and acne are not mutually exclusive, however, which means you can have both simultaneously. For instance, you can have hives on the face and acne on the shoulders at the same time.
References
- Hives. American Academy of Dermatology (2018). https://www.aad.org/public/diseases/itchy-skin/hives#overview
- Greiwe, J. & Bernstein, J. A. Approach to the patient with hives. Med Clin North Am. 104, 15-24 (2020). https://pubmed.ncbi.nlm.nih.gov/31757233/
- Urticaria (hives). NHS Inform (2019). https://www.nhsinform.scot/illnesses-and-conditions/skin-hair-and-nails/urticaria-hives#about-urticaria-hives
- Urticaria. National Skin Centre (2016). https://www.nsc.com.sg/Patient-Guide/Health-Library/Types of Skin Conditions/Pages/Urticaria.aspx
- Antia, C., Baquerizo, K., Korman, A., Bernstein, J. A. & Alikhan, A. Urticaria: A comprehensive review: Epidemiology, diagnosis, and work-up. J Am Acad Dermatol. 79, 599-614 (2018). https://pubmed.ncbi.nlm.nih.gov/30241623/
- Saini, S. S. & Kaplan, A. P. Chronic spontaneous urticaria: The devil’s itch. J Allergy Clin Immunol Pract. 6, 1097-1106 (2018). https://pubmed.ncbi.nlm.nih.gov/30033911/
The post Hives (Urticaria) appeared first on Acne.org.
