Rosacea Symptoms and Treatment

The Essential Info
Rosacea is a chronic skin condition that affects about 5% of people over 30 years old, particularly women and people with fair skin.
Rosacea may sometimes look similar to acne, but it is a different disease and requires different treatment.
Symptoms most commonly include:
- Sustained flushing of the center area of the face
- Papules & pustules, which are red and inflamed lesions that resemble pimples
- Dilated blood vessels
The following symptoms may also be present:
- Burning/stinging sensation
- Elevated red plaques
- Dry appearance to skin
- Swelling
- Burning or itching eyes, eyelid inflammation, styes, eye redness
- Thickened bulbous growths on the nose (usually in men)
Prevention and symptom relief:
- Wear sunscreen
- Avoid irritating products such as soap, astringents, toners, menthol, and camphor

The Science
What Is Rosacea?
Rosacea, also referred to as acne rosacea, is different from acne vulgaris, which is what normally affects younger people. Rosacea affects mostly adults over the age of 30, with a higher incidence in women.1,2 People with fair skin are more often affected, although darker skin types may also experience symptoms.2
Rosacea is fairly common (worldwide estimates average about 5% of people), and while its symptoms may wax and wane, it is most often referred to as a chronic condition. Rosacea is usually a progressive disease, and without treatment may continue to worsen over time. Because it affects appearance, rosacea can also cause emotional repercussions.
Comparing Rosacea and Acne
One recent study compared the symptoms of rosacea and acne. The researchers looked at a total of 463 females with rosacea and 412 females with acne. They found that, compared to females with acne, females with rosacea had:
- A different pattern of skin redness
- More skin burning, dryness, and itching
- A weaker skin barrier, meaning skin that is more prone to drying out and vulnerable3
Expand to read details of study

The study was published in the Pakistan Journal of Medical Sciences in 2016. The researchers looked at 463 females with rosacea, 412 females with acne, and 400 females without either disease. The females were 20 to 50 years old with an average age of 30 years old. The researchers summarized their conclusions as follows: “[Redness], burning, dryness and itching are the characteristics of papulopustular rosacea, which makes it different from acne vulgaris. The [skin] barrier function was damaged in papulopustular rosacea patients while not impaired in that of acne vulgaris patients.”3
Symptoms of Rosacea
Flushing
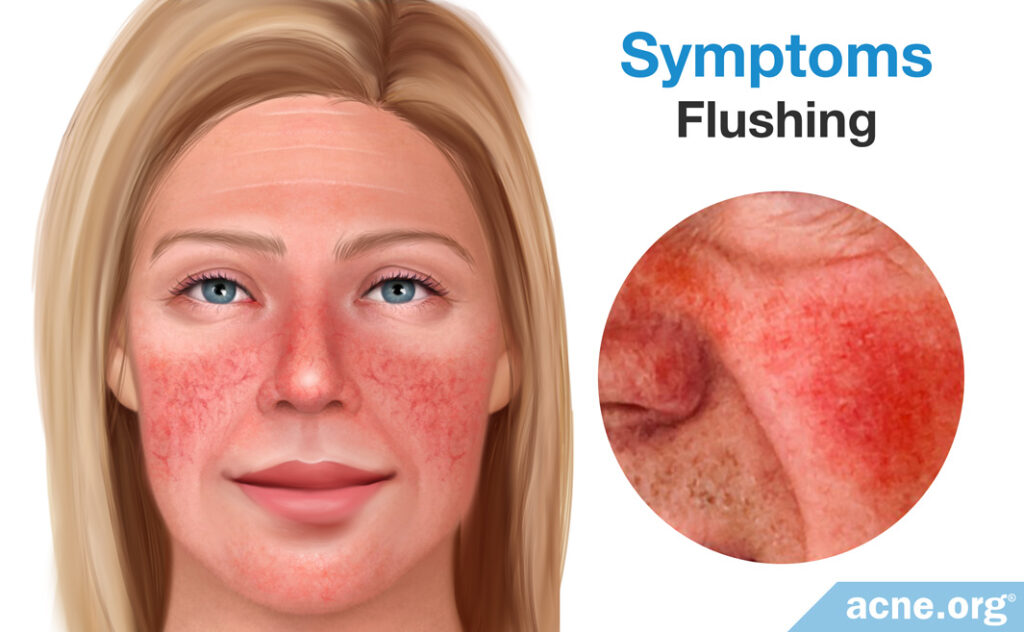
The most common sign of rosacea is frequent or sustained blushing or flushing of the skin. The skin of the central face appears red and inflamed. In women, this is not to be confused with monthly flushing before menstruation.
Papules / Pustules
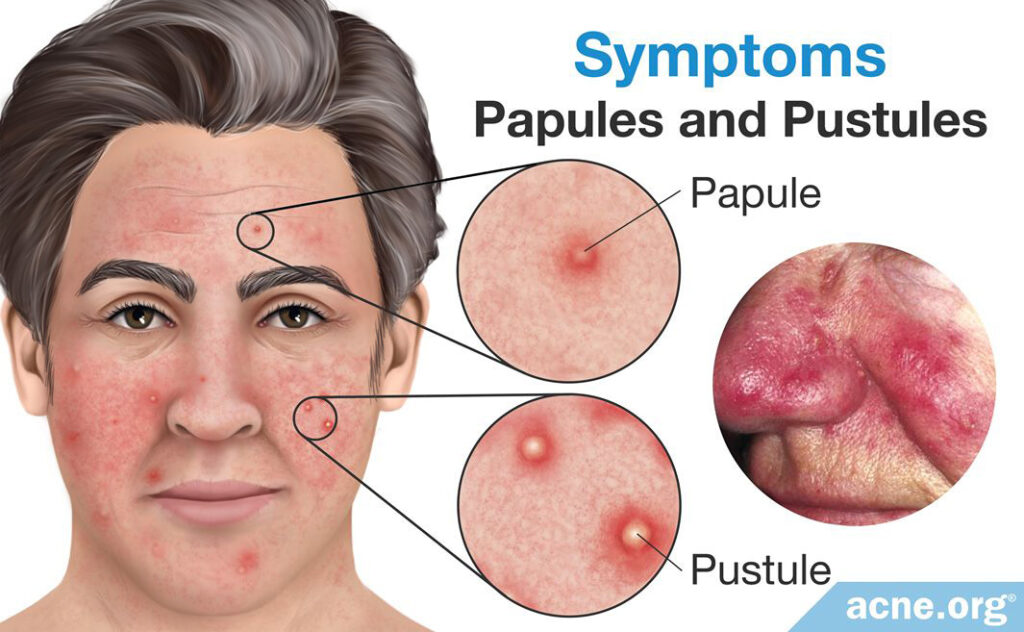
Red, inflamed lesions that may or may not have a white/yellow center. Rosacea does not include non-inflamed whiteheads or blackheads, although one can have rosacea and acne vulgaris simultaneously, so whiteheads or blackheads may be present if this is the case.
Dilated Blood Vessels
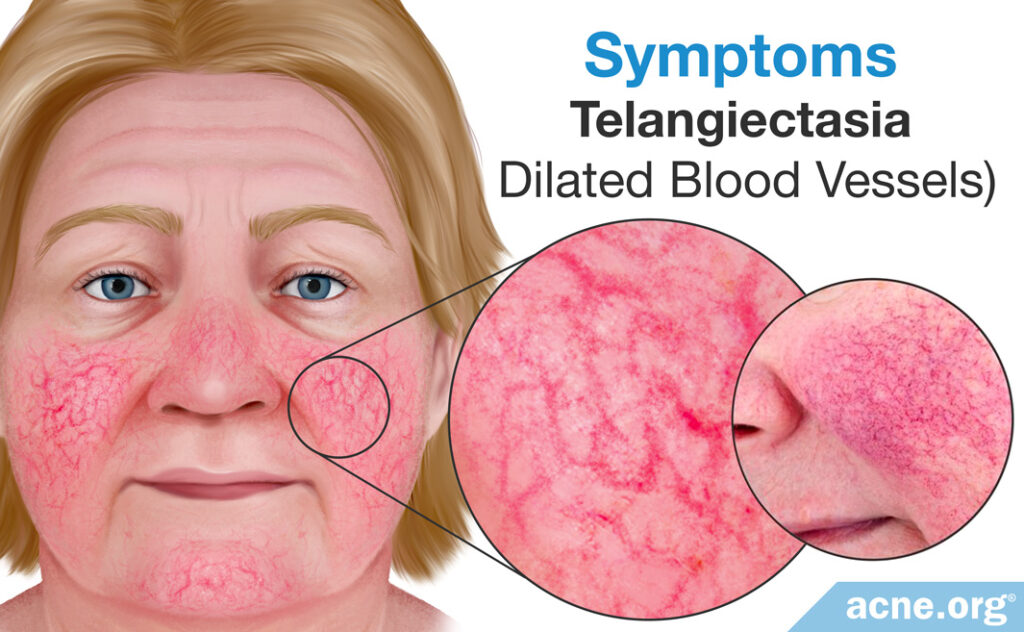
Called telangiectasia, these dilated blood vessels resemble small squiggles on the surface of the skin. They may be obvious or they may be hidden by the redness of the surrounding skin.
Rosacea Symptoms May Also Include Any Combination of the Following:
- Burning or stinging sensation to the skin
- Elevated red plaques
- Dry appearance to the skin
- Fluid under the skin – edema
- Burning or itching eyes, eyelid inflammation, styes, red eyes
- Skin thickening, bulbous growths, rhinophyma2-6
Rosacea Is Often Confused With:
- Acne vulgaris
- Seborrheic dermatitis
- Seborrhea
- Keratosis pilaris
- Demodicosis
- Pyoderma faciale
- Steroid-induced acneiform eruptions
- Perioral dermatitis
Diagnosis
Physicians experience a challenge when diagnosing rosacea because of the numerous ways it can present itself. The National Rosacea Society has broken rosacea into four main categories:2-4
#1 Erythematotelangiectatic
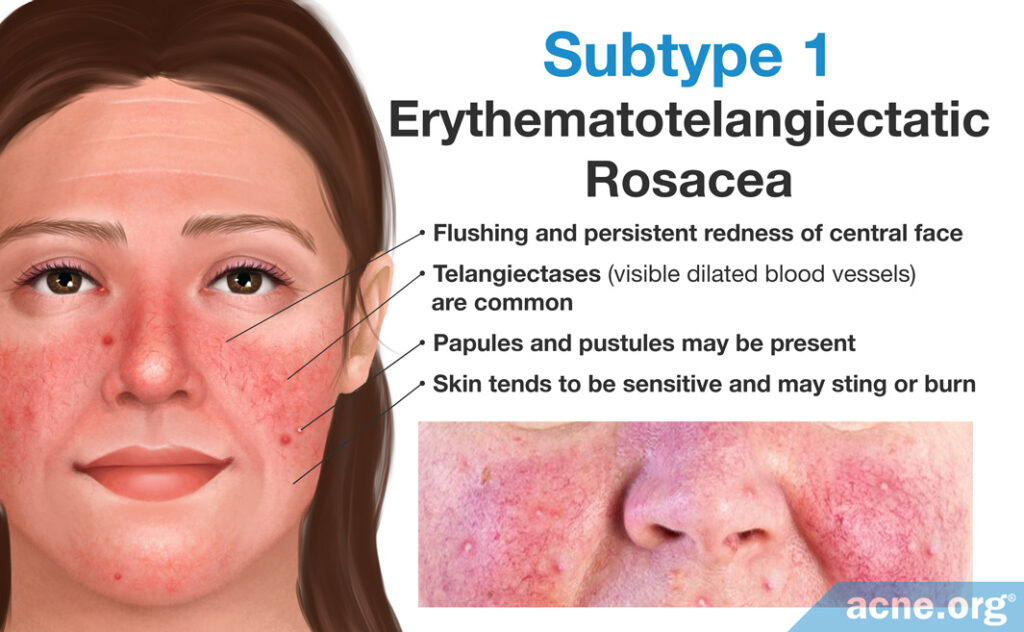
- Burning or stinging sensation to the skin
- Characterized by flushing and redness
- May also include burning, stinging, roughness, and scaling
- Some dilated blood vessels may be present
#2 Papulopustular
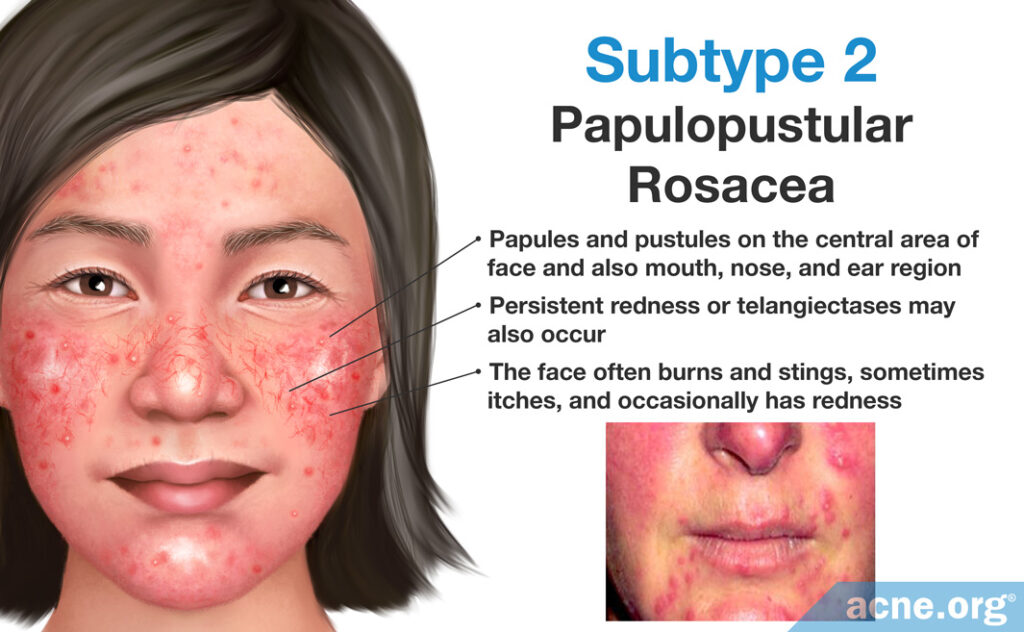
- Characterized by redness with papules and pustules present
- May resemble acne vulgaris, but no comedones are present (unless the person has acne vulgaris simultaneously)
- Burning and stinging may be present
- Some dilated blood vessels may be present
#3 Phymatous
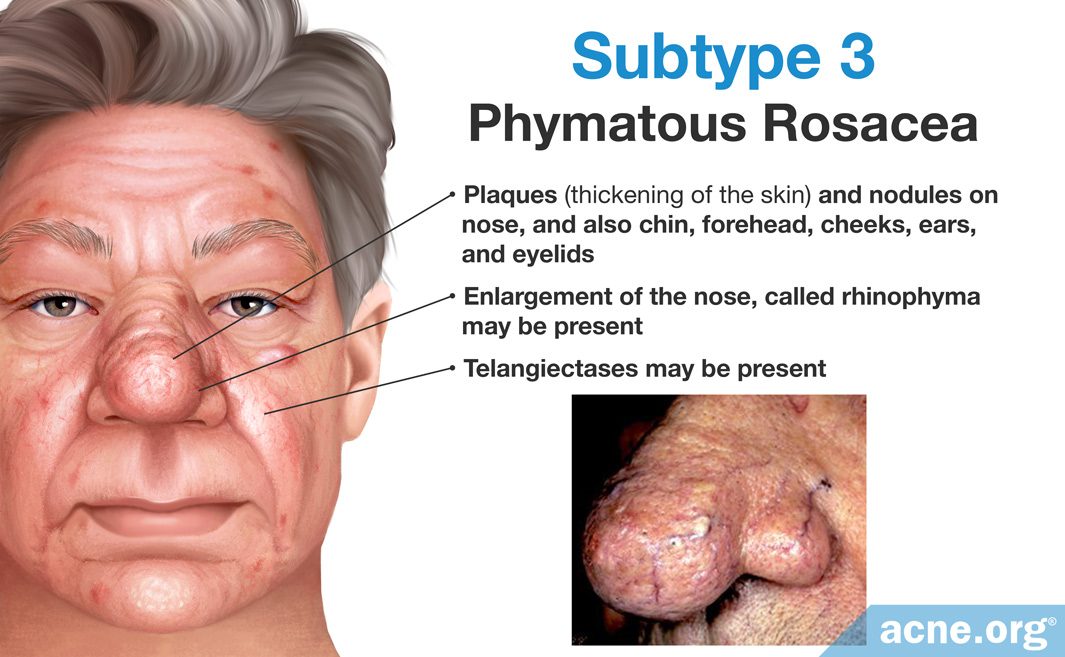
- Thickening of skin
- Irregularities of skin surface, bumpy appearance
- Rhinophyma: thickening of skin on the nose, resulting in an irregular, bumpy appearance
- Dilated blood vessels
#4 Ocular
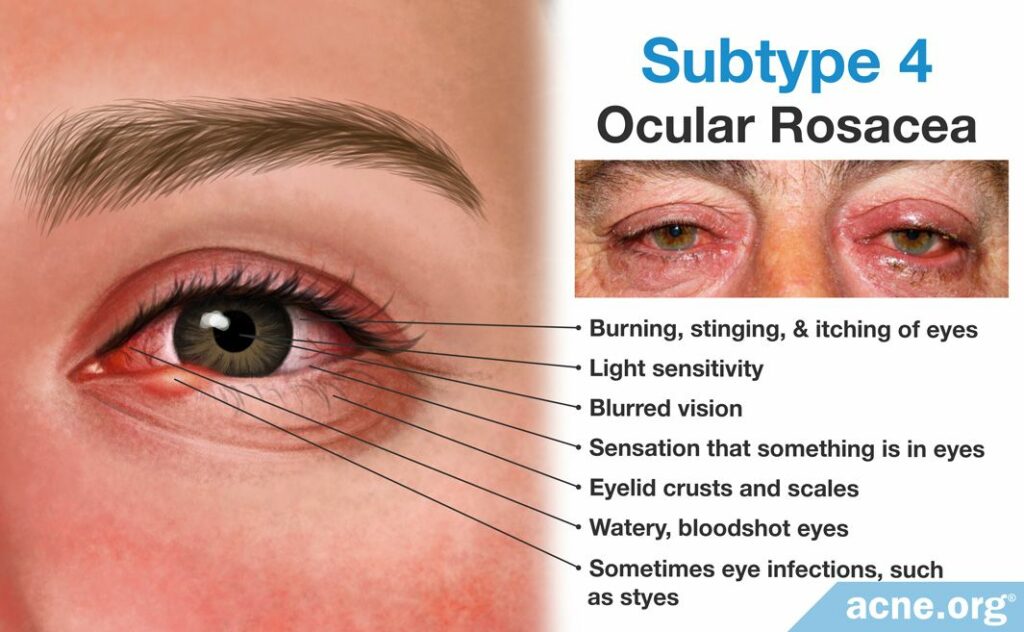
- May include any of the following eye symptoms: watery, bloodshot, burning/stinging, itching, lid redness, stye, light sensitivity, blurred vision, foreign body sensation
- Ocular rosacea is usually present in conjunction with other signs of rosacea on the skin, however, skin symptoms are not required
- Treatment may require topical as well as ophthalmologic treatment
However, doctors and scientists are starting to recognize that a person’s rosacea symptoms don’t always fall neatly into just one of these four subtypes and can also change over time. Therefore, an international expert panel called the global ROSacea COnsensus (ROSCO) recently recommended that, instead of relying on subtype classifications, doctors should treat rosacea on a case-by-case basis. The ROSCO panel published their recommendations in the British Journal of Dermatology in 2020.7
Treatments
According to a thorough and informative 2009 Review on Rosacea published by Thomas Jefferson University (Jefferson Medical College), “…the cure for rosacea remains elusive, and all currently used medications are for symptomatic control only. No precise treatment algorithm has become the standard of care; treatment remains empirical.”1 This may sound ominous, but in reality, we have several methods of tackling rosacea which are proven effective.
Common treatments
- Metronidazole (MetroGel, MetroCream)
An often prescribed treatment, studies show this topical antibiotic providing superior results to placebo.1-2 [72% reduction in rosacea lesions, 45% redness reduction, statistically significant improvement in dilated blood vessels.] - Azelaic acid (Azelex)
Studies have shown effectiveness [73.4% reduction in rosacea lesions, significant redness reduction, no improvement in dilated blood vessels] with concentrations up to 20%. 15% is standard.3-5 - Sodium sulfacetamide 10% and sulfur 5% (Sulfacet)
Studies hint toward good results.6 [80% reduction in rosacea lesions, 69% redness reduction. No data on dilated blood vessels.] - Benzoyl peroxide or benzoyl peroxide + clindamycin (Benzaclin)
Trial results from benzoyl peroxide administration show significant improvement in rosacea lesions,7 but no improvement in dilated blood vessels. [Benzoyl peroxide + clindamycin shows a 71.3% reduction in rosacea lesions, and significant redness reduction.8-9 No data regarding dilated blood vessels for benzoyl peroxide + clindamycin.] - Accutane (isotretinoin)
This is particularly effective for younger patients and also those with phymatous rosacea.10 - Oral antibiotics (most notably minocycline & doxycycline)
Patient and doctor should be in close contact and limit exposure to short-term therapy (no longer than one year). [1.5% minocycline foam, which was approved in May 2020, reduced lesion counts in patients with moderate-to-severe papulopustular rosacea by 61%, while 52.1% of patients achieved treatment success (clear face). No data on dilated blood vessels.]11 [Results from doxycycline trials show a 48%-59% improvement in rosacea lesions. No evidence of reduction in dilated blood vessels.]12 - IPL (Intense pulsed light) and long-pulsed dye lasers
These machines provide treatments that can help with redness and dilated blood vessels, but are impermanent solutions. - Regular ophthalmologist care for eye symptoms
Be sure to see your ophthalmologist if you suspect ocular rosacea.
Less Common Treatments
- Oral nicotinamide + zinc (Nicomide, Nic/Zn)
[79% of patients showed moderately better or much better improvement in appearance (based on patient global evaluation) after 4 weeks of treatment.]13 - Hormonal treatment – Spironolactone, Prednisone, Oral Contraceptives14
- Mite, parasite, fungal treatment – Permethrin cream (Nix), Ivermectin (Stromectol)15, Crotamiton (Eurax), Ketoconazole (Nizoral)
- Alpha blockers
Experimental Treatments
- Rifaximin (SIBO treatment)
An interesting study in the journal Clinical Gastroenterology and Hepatology showed a much higher prevalence of intestinal bacteria (SIBO) in people with rosacea than those without. Patients were given Rifaximin, an antibiotic which does not penetrate the intestinal wall, effectively reducing or eradicating SIBO. After SIBO was controlled, 20 of 28 patients cleared completely, and 6 more greatly improved. Results lasted for at least 9 months at follow-up.16 - Minocycline extended-release capsules (DFD-29 40 mg)
A study that included 205 patients with rosacea found that 16 weeks of daily treatment with minocycline extended-release capsules led to clearing or near-clearing of rosacea symptoms in 66% of patients.11 - Encapsulated benzoyl peroxide cream
One study that included 90 patients with rosacea found that 12 weeks of treatmetn with 5% encapsulated benzoyl peroxide led to a significant improvement in rosacea symptoms in 56% of patients.17
Other Things You Can Do to Help Your Symptoms
- Wear sunscreen: Sunscreen is an important adjunct to rosacea care.18 Pharmaceutical manufacturers incorporate sunscreen into prescription preparations at times. Zinc oxide is an effective broad spectrum sunscreen ingredient that seems to be well tolerated by people with rosacea.
- Avoid: Products that strip or irritate the skin such as soap (use soap-free cleanser instead), sodium lauryl sulfate (avoid cleansers with this ingredient), astringents, toners, menthol, and camphor.
Finding a Doctor
Because of its wide ranging symptoms, rosacea can easily be confused with other conditions. Be sure to educate yourself and be your own advocate when speaking to a medical professional.
When choosing a doctor, be certain to find someone experienced in treating patients with rosacea (this will often mean a dermatologist). Then don’t be afraid to ask some tough questions such as:
- Are you certain what I have is rosacea and not a similar condition?
- How many patients with rosacea have you treated?
- What is the effectiveness of the treatments you’ve prescribed? Why have you decided on this treatment for my particular case?
Most importantly, trust your gut. Your dermatologist’s diagnosis and strategy for treatment should be strong and confident. If you feel uncomfortable, simply visit another dermatologist. Very often with dermatology as well as with other conditions, a second or third opinion is incredibly valuable.
Then, once your doctor prescribes a treatment protocol, stick with it closely and orchestrate regular follow-up visits. If you do not improve, a second opinion may be in order.
References
What Is Rosacea?
- Berg, M. & Liden, S. An epidemiological study of rosacea. Acta Derm. Venereol. 69, 419-23 (1989). https://www.ncbi.nlm.nih.gov/pubmed/2572109
- Wilkin. J. et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J. Am. Acad. Dermatol. 46, 584-7 (2002). https://www.ncbi.nlm.nih.gov/pubmed/11907512
- Zhou, M., Xie, H., Cheng, L. & Li, J. Clinical characteristics and epidermal barrier function of papulopustular rosacea: A comparison study with acne vulgaris. Pak. J. Med. Sci. 32, 1344 – 1348 (2016). https://pubmed.ncbi.nlm.nih.gov/28083023/
- Wilkin, J. et al. Standard grading system for rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J. Am. Acad. Dermatol. 50, 907-912 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15153893
- Goldgar, C., Keahey, D. J. & Houchins, J. Treatment options for acne rosacea. Am. Fam. Physician 80, 461-468 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19725487
- Del Rosso, J. Q., Baldwin, H. & Webster, G. American Acne & Rosacea Society rosacea medical guidelines. J. Drugs Dermatol. 7, 531-533 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18561582
- Schaller, M., Almeida, L. M. C., Bewley, A., Cribier, B., Del Rosso, J., Dlova, N. C., Gallo, R. L., Granstein, R. D., Kautz, G., Mannis, M. J., Micali, G., Oon, H. H., Rajagopalan, M., Steinhoff, M., Tanghetti, E., Thiboutot, D., Troielli, P., Webster, G., Zierhut, M., van Zuuren, E. J. & Tan, J. Recommendations for rosacea diagnosis, classification and management: update from the global ROSacea COnsensus 2019 panel. Br. J. Dermatol. 182, 1269-1276 (2020). https://pubmed.ncbi.nlm.nih.gov/31392722/
Treatments:
- Culp, B. & Scheinfeld, N. Rosacea: a review. P. T. 34, 38-45 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19562004
- Tan, J. K. et al. Randomized placebo-controlled trial of metronidazole 1% cream with sunscreen SPF 15 in treatment of rosacea. J. Cutan. Med. Surg. 6, 529-534 (2002). https://www.ncbi.nlm.nih.gov/pubmed/12001006
- Bjerke, R., Fyrand, O. & Graupe, K. Double-blind comparison of azelaic acid 20% cream and its vehicle in treatment of papulo-pustular rosacea. Acta Derm. Venereol. 79, 456-459 (1999). https://www.ncbi.nlm.nih.gov/pubmed/10598760
- Gupta, A. K. & Gover, M. D. Azelaic acid (15% gel) in the treatment of acne rosacea. Int. J. Dermatol. 46, 533-538 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17472690
- Liu, R. H., Smith, M. K., Basta, S. A. & Farmer, E. R. Azelaic acid in the treatment of papulopustular rosacea: a systematic review of randomized controlled trials. Arch. Dermatol. 142, 1047-1052 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16924055
- Torok, H. M. et al. Combination sodium sulfacetamide 10% and sulfur 5% cream with sunscreens versus metronidazole 0.75% cream for rosacea. Cutis 75, 357-363 (2005). https://www.ncbi.nlm.nih.gov/pubmed/16047874
- Montes, L. F., Cordero, A. A., Kriner, J., Loder, J. & Flanagan, A. D. Topical treatment of acne rosacea with benzoyl peroxide acetone gel. Cutis 32, 185-190 (1983). https://www.ncbi.nlm.nih.gov/pubmed/6225627
- Breneman, D. et al. Double-blind, randomized, vehicle-controlled clinical trial of once-daily benzoyl peroxide/clindamycin gel in the treatment of patients with moderate to severe rosacea. Int. J. Dermatol. 43, 381-387 (2004). https://www.ncbi.nlm.nih.gov/pubmed/15117375
- Kapes, B. P. acnes possible factor in rosacea: BenzaClin a significant Tx in lesion reduction. Dermatology Times. 1 Apr. 2003.
- Hoting, E., Paul, E. & Plewig, G. Treatment of rosacea with isotretinoin. Int. J. Dermatol. 46, 533-538 (2007). https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-4362.1986.tb04533.x
- van Zuuren, E. J., Arents, B. W. M., van der Linden, M. M. D., Vermeulen, S., Fedorowicz, Z. & Tan, J. Rosacea: New concepts in classification and treatment. Am. J. Clin. Dermatol. 22, 457-465 (2021). https://pubmed.ncbi.nlm.nih.gov/33759078/
- Del Rosso, J. Q. et al. Two randomized phase III clinical trials evaluating anti-inflammatory dose doxycycline (40-mg doxycycline, USP capsules) administered once daily for treatment of rosacea. J. Am. Acad. Dermatol. 56, 791-802 (2007). https://www.ncbi.nlm.nih.gov/pubmed/17367893
- Fivenson, D. P. The mechanisms of action of nicotinamide and zinc in inflammatory skin disease. Cutis 77, 5-10 (2006). https://www.ncbi.nlm.nih.gov/pubmed/16871773
- Jansen, T., Plewig, G. & Kligman, A. M. Diagnosis and treatment of rosacea fulminans. Dermatology 188, 251-254 (1994). https://www.karger.com/Article/Abstract/247160
- Dursun, R., Daye, M. & Durmaz, K. Acne and rosacea: What’s new for treatment? Dermatol, Ther. 32, e13020 (2019). https://pubmed.ncbi.nlm.nih.gov/31294907/
- Parodi, A. et al. Small intestinal bacterial overgrowth in rosacea: clinical effectiveness of its eradication. Clin. Gastroenterol. Hepatol. 6, 759-764 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18456568
- Leyden, J. J. Randomized, phase 2, dose-ranging study in the treatment of rosacea with encapsulated benzoyl peroxide gel. J. Drugs Dermatol. 13, 685-688 (2014). https://pubmed.ncbi.nlm.nih.gov/24918558/
- Goldgar, C., Keahey, D. J. & Houchins, J. Treatment options for acne rosacea. Am. Fam. Physician 80, 461-468 (2009). https://www.ncbi.nlm.nih.gov/pubmed/19725487
