A Common Skin Condition, Particularly in Young Children, that Includes Itchy, Dry, and Scaly skin, Typically on the Cheeks, Arms, and Legs

The Essential Info
Eczema, also called atopic dermatitis, is a chronic skin condition that causes dry, itchy, and cracked skin.
It normally begins before the age of 5, but continues in about 1/2 of cases–usually in a milder form–into adulthood.
Genetics play a role in the development of eczema, particularly a mutation in the gene responsible for producing a protein called filaggrin, which is an important part of our skin’s protective barrier.
No cure exists, but some self-care measures can help, such as:
- Applying a moisturizer regularly
- Using an over-the-counter anti-itch cream
- Reducing stress
- Avoiding triggers such as soaps and harsh cleansers/detergents, long hot showers, allergens (i.e. pollen, dust mites, mold)
It is important to be patient and persevere with your self-care. It often takes trial and error to figure out what works best for your skin, but persistence can pay off with significantly improved symptoms.
If self-care measures are not enough, your doctor may recommend a more potent prescription medication, but many of these come with side effects, so be sure to ask your dermatologist for a full list of side effects and discuss the decision with him/her thoroughly.
Eczema Vs. Acne: Eczema and acne are completely different conditions, and diagnosis and treatment are unique to each.

The Science
Eczema, medically known as atopic dermatitis, is a long-lasting skin condition affecting all ethnicities that causes itchy, dry, and scaly skin, typically on the cheeks, arms, and legs.
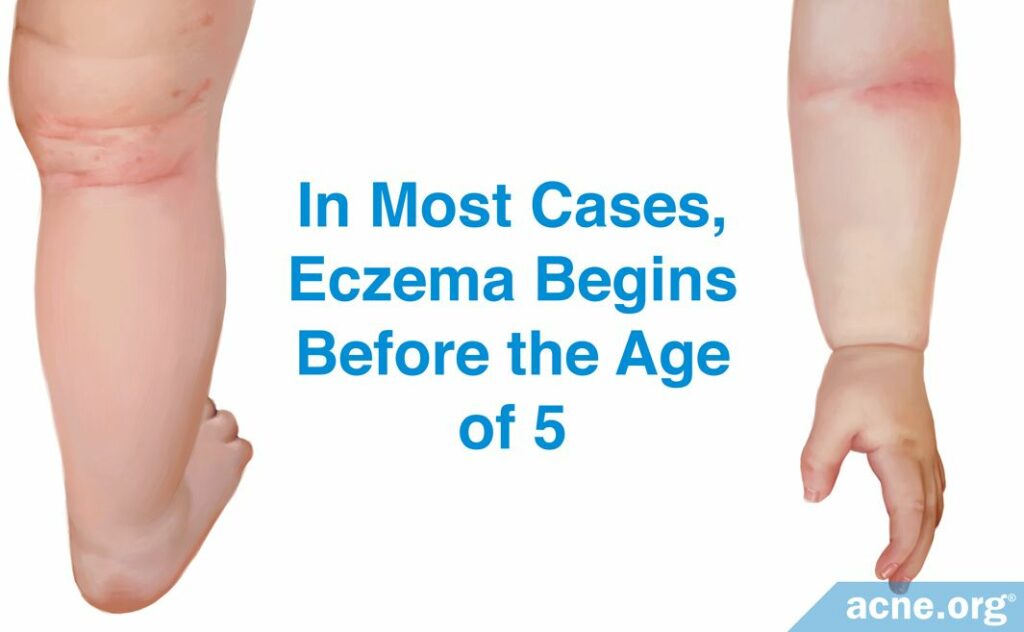
In 90% of cases, eczema presents before the age of 5 years, sometimes as early as the second month of life.1 Eczema that starts in adulthood is rare but possible.
Approximately 10% of people experience eczema at some point in their life,2 with females experiencing symptoms slightly more often than males.
Symptoms
Signs and symptoms may include:
- Dry skin
- Itching
- Redness
- Small, raised bumps, which leak fluid and form crusts if scratched. Typically, the bumps develop on the cheeks and in the creases of the elbows and knees.
- Thick, cracked, scaly skin
If the skin becomes infected with bacteria, small, yellowish, pus-filled bumps called pustules may develop.
Eczema can occur anywhere on the skin. The most common locations include:
- Cheeks
- Arms
- Legs
Eczema is a chronic condition, which means it often persists for months and even years. The symptoms may go away for a time before striking back. About half of individuals who had eczema in childhood continue to have symptoms as adults, although the symptoms tend to get milder.
Causes of Eczema
The exact cause of eczema is unclear, but we know that genetics play a role. People with eczema have a mutation in the gene responsible for producing a protein called filaggrin.3 Filaggrin is an essential building block in our skin’s protective barrier–the epidermis. The epidermis preserves the skin integrity, keeping a healthy level of moisture inside and bacteria, viruses, and harmful chemicals–outside. A lack of filaggrin, as it is the case in people with eczema, allows moisture to escape the skin and weakens the skin’s protective barrier.
Eczema often occurs in more than one family member. For instance, there is an approximately 50% likelihood of a child developing eczema if one of their parents has it.2
Research suggests that environmental factors such as air pollution and exposure to ozone and cigarette smoke may also contribute to the development of eczema.4
Children with eczema also often have one or more of these conditions:
- Asthma
- Hay fever
- Food allergies, particularly to: Nuts, Shellfish, and Milk/Dairy.
Diagnosis
Your doctor will diagnose the condition by closely looking at the affected skin and asking questions about your symptoms. No tests are usually required.
However, in some cases, the doctor may administer a patch test if he suspects that some other disease (e.g., allergic contact dermatitis) is causing your symptoms or that you have an allergy (e.g., to milk) that aggravates them.
What Is a Patch Test? Adhesive patches with small amounts of different allergens on them are applied to your back. The patches remain on your skin for 2-3 days, after which the doctor checks if any of the patches produced a skin reaction. If a patch with a certain allergen triggers a reaction, it is likely that this allergen causes or aggravates eczema.
Treatment
You cannot cure eczema, but you can learn to control the symptoms. Eczema is a stubborn, long-lasting condition. It may take months and even years before you figure out what works best for your, or your child’s, symptoms, and even after successful treatment the symptoms may return. It is crucial to be patient and consistent with your skin care. Some of these self-care measures can help:5
- Apply moisturizers at least 2-3 times a day. Dry skin worsens the symptoms, and moisturizers will help to keep the skin moisturized throughout the day.
- Avoid soaps. Soaps are known to dry the skin. Opt for gentle, moisturizing cleansers instead. Look for scent-free cleansers, as fragrances are more likely to irritate the skin.
- Avoid long, hot showers. Hot water causes your skin to lose moisture after a shower more quickly.
- See if you can pay attention to what worsens your symptoms and try to avoid the triggers. Some of the common triggers include:
- Chemical irritants such as: Laundry detergent, shampoo, surface cleaner, hand and dish soap, cold temperatures, hot temperatures, sweating, environmental allergens like pollen, dust mites, mold, and stress.
- Use an over-the-counter hydrocortisone cream to relieve itching up to twice a day, reducing the frequency as your symptoms improve.
- Don’t scratch the affected skin. Wear comfortable, breathable apparel and avoid itchy fabrics like wool.
- Take a lukewarm (not hot!) bath. Add a quarter-cup of baking soda or a half-cup of regular household bleach per full bathtub. Soak for up to 10 minutes, then rinse off, and gently dry your skin with a soft towel. Apply a moisturizer immediately afterwards. Soaking in lukewarm water helps your skin absorb moisture, and adding baking soda or bleach may help to lessen inflammation. In addition, bathing helps to relax and relieve stress. Remember to moisturize your skin immediately after and no hot water. Taking a bath 2-3 times a week is about right. Note: People who are sensitive to bleach or have asthma should consult with a doctor first.
- If you need to handle something that you know can irritate your skin, apply a barrier cream first. This type of cream can be as simple as petroleum jelly (Vaseline®), although there are fancy brand-name barrier creams on the market as well. The goal is to coat your hands with the cream like an invisible glove so that the irritant substance doesn’t come into direct contact with your skin.
If self-care measures are not enough, your doctor may prescribe one or several of the following treatments:
Topical corticosteroids: Creams or ointments containing corticosteroids help to control itching and reduce inflammation. Prescription creams are more potent than their over-the-counter alternatives and should be used strictly as prescribed. An overuse can cause side-effects, such as:
- Thinning or thickening of the skin
- Skin darkening
- Stretch marks
The less common, but more dangerous side-effects include:
- Eye problems (e.g., glaucoma and cataract)
- Acne
- Folliculitis
- Adrenal suppression
Topical calcineurin inhibitors: The body’s immune response is what causes itching and redness in eczema. Creams containing calcineurin inhibitors such as tacrolimus or pimecrolimus inhibit this immune response, which will lessen itching and redness. Note: A few patients receiving pimecrolimus were diagnosed with skin cancer or lymphoma (a type of blood cancer), although it is unlikely that cancer was a side-effect caused by the drug.2
The most common side-effects of calcineurin inhibitors include:
- Burning
- Stinging
Topical antibiotics: Your doctor may prescribe antibiotic creams to treat or prevent bacterial infection of the skin.
The most common side-effects of topical antibiotics include:
- Rash
- Burning
- Stinging
Biologic drugs: The U.S. Food and Drug Administration (FDA) has recently approved the first genetically engineered (containing human DNA) medication for moderate-to-severe eczema, called dupilumab (Dupixent®). Dupilumab blocks the immune response and reduces symptoms such as itching and redness.
The most common side-effects of dupilumab include:
- Conjunctivitis (pink eye)
- Cold sores on the lips and mouth
- Inflammation at the site of injection
Light therapy: Light therapy, also called phototherapy, literally means treatment with a special kind of light. It may be recommended if topical medications are ineffective.
One study found that for children who received 10 or more sessions of light therapy, eczema completely cleared in half of cases, and half of those remained clear for a year after stopping light treatment.6
The most common side-effects of light therapy include:
- Sunburn
- Skin aging
Oral corticosteroids: Reserved for the most severe cases. Generally, not recommended due to serious side-effects such as:
- Mood swings
- Blurred vision
- Muscle weakness
- Easy bruising
- Swelling
- Osteoporosis (bone weakness)
- Acne
- Eye problems
Eczema Vs. Acne
Eczema and acne are different, unrelated conditions. Your doctor will easily differentiate one from another by looking at your skin.
Eczema and acne are not mutually exclusive, which means you can have both simultaneously. For instance, you can have eczema on the face and acne on the back.
Summary
Eczema is a chronic skin condition that causes dry, itchy, and cracked skin. No cure exists, but taking self-care measures like applying a moisturizer, avoiding triggers, and using an over-the-counter anti-itch cream can help to relieve symptoms. If self-care measures are insufficient, your doctor may recommend a more potent prescription medication.
With eczema, it is important to be patient and persevere with your skin care. It may take time before you figure out what works best for your skin, but if you are persistent, you can significantly improve your symptoms and prevent the disease from deteriorating.
References
- Eczema. American Academy of Dermatology (2018). https://www.aad.org/public/diseases/eczema/atopic-dermatitis#overview
- Eczema. National Eczema Association (2019). https://nationaleczema.org/eczema/types-of-eczema/atopic-dermatitis/
- O’Regan, G. M., Sandilands, A., McLean, W. H. I. & Irvine, A. D. Filaggrin in eczema. Journal of Allergy and Clinical Immunology 122, 689 – 693 (2008). https://www.ncbi.nlm.nih.gov/pubmed/18774165
- Puri, P., Nandar, S. K., Kathuria, S. & Ramesh, V. Effects of air pollution on the skin: A review. Indian J Dermatol Venereol Leprol. 83, 415-423 (2017). https://pubmed.ncbi.nlm.nih.gov/28195077/
- Guarneri, F., Belloni Fortina, A., Corazza, M., Cristaudo, A., Foti, C., Parodi, A., Pigatto, P., Stingeni, L. & DE Pità, O. Topical non-pharmacological treatment of eczema: an Italian consensus. Ital J Dermatol Venerol. 157, 402-413 (2022). https://pubmed.ncbi.nlm.nih.gov/36213968/
- Hunjan, M. K., Brockley, J. R., Buka, R. & Ramesh, R. Treatment of paediatric eczema with narrowband ultraviolet light B therapy. Photodermatol Photoimmunol Photomed. 37, 105-110 (2021). https://pubmed.ncbi.nlm.nih.gov/33012054/
The post Eczema (Atopic Dermatitis) appeared first on Acne.org.
